In the era of digital healthcare transformation, the question “what is EMR systems?” has become more relevant than ever. From clinics to large hospitals, the adoption of Electronic Medical Record (EMR) systems is reshaping how medical professionals manage patient information, streamline workflows, and improve quality of care.
This comprehensive guide will walk you through the fundamentals of EMR systems: definitions, features, benefits, challenges, use cases in healthcare, comparisons with EHR systems, and future trends. Additionally, we will showcase how HBLAB provides world-class EMR system development and customization services, delivering cost-effective, secure, and scalable solutions for global healthcare providers.
What is EMR Systems?
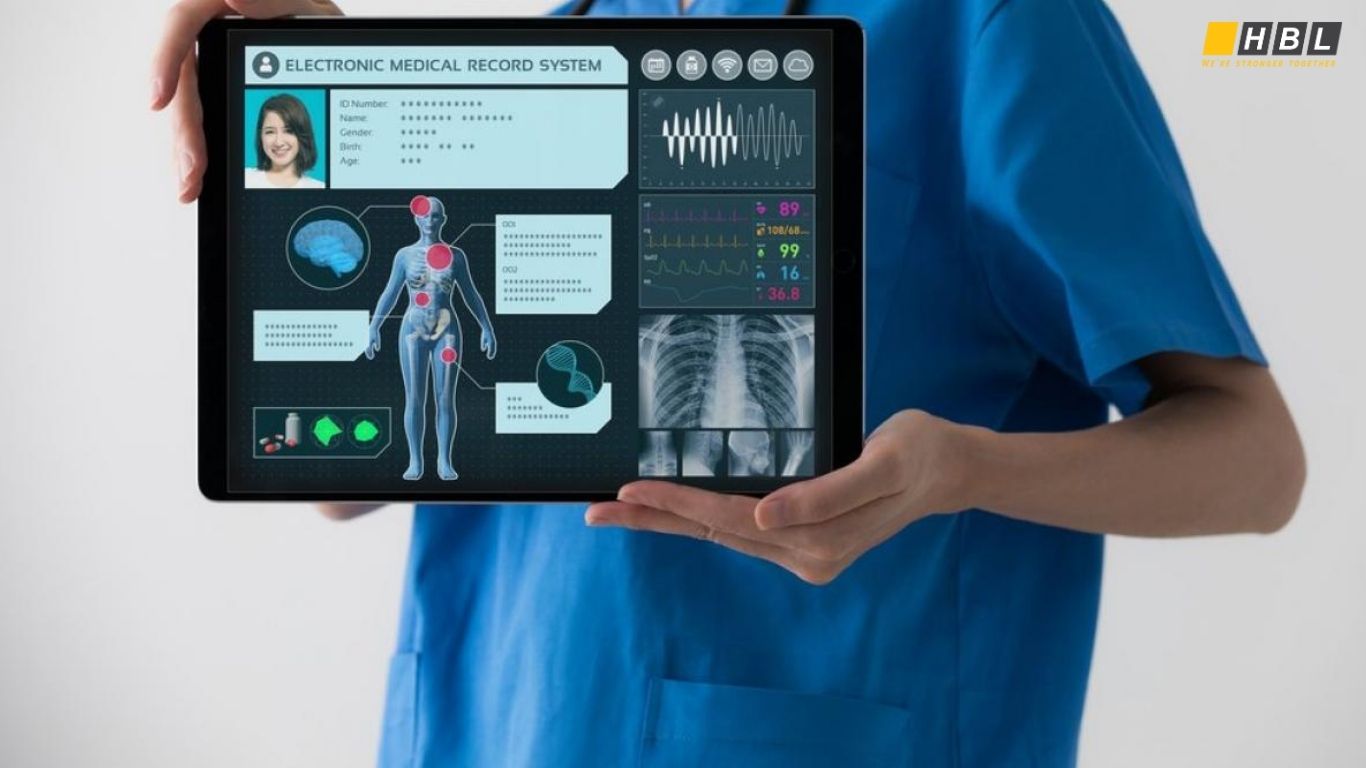
An Electronic Medical Record (EMR) system is a digital version of a patient’s paper chart. It contains real-time patient records, including medical history, diagnoses, medications, treatment plans, immunization dates, allergies, lab test results, and physician notes.
Unlike traditional paper-based files, EMR systems enable healthcare professionals to access patient data quickly, reduce errors, and improve decision-making.
In short:
- EMR = digital medical chart for use within a single healthcare organization.
- Designed mainly for internal clinical use, not for sharing across multiple organizations.

What is EMR Systems in Healthcare?
In healthcare, EMR systems act as the backbone of digital patient care. They:
- Store and organize patient data.
- Provide physicians with decision support.
- Facilitate billing and insurance claims.
- Improve efficiency by reducing paperwork.
- Ensure regulatory compliance.
Hospitals and clinics worldwide are adopting EMR systems to replace manual charting and ensure accurate, up-to-date medical records.
Key Features of EMR Systems
When asking “what is EMR systems?”, it’s important to understand their core features. A modern EMR platform goes far beyond digital record-keeping. It provides healthcare providers with powerful tools to streamline workflows, improve patient safety, and ensure regulatory compliance.
1. Centralized Patient Record Management
All patient information—including demographics, medical history, allergies, medications, lab results, and physician notes—is stored in a single, digital profile. This eliminates duplication, ensures consistency, and enables quick access during consultations.
2. Clinical Decision Support (CDS)
EMR systems include built-in alerts and reminders that help clinicians avoid errors, such as drug interactions or missed follow-up appointments. CDS tools also provide evidence-based guidelines to support better treatment decisions.
3. E-Prescribing
Doctors can send prescriptions directly to pharmacies through the EMR system. This reduces handwriting errors, improves patient convenience, and streamlines medication management.
4. Laboratory and Imaging Integration
Test orders and diagnostic results are directly connected to the patient’s EMR. Physicians can view lab reports, X-ray images, and pathology results in real time without relying on separate systems.
5. Appointment Scheduling and Workflow Automation
Most EMR systems come with scheduling modules that reduce no-shows and optimize physician availability. Automated reminders via SMS or email further enhance patient engagement.
6. Billing and Insurance Integration
EMRs often include medical billing tools, allowing hospitals to generate claims, verify insurance eligibility, and track reimbursements. This ensures smoother revenue cycle management.
7. Data Analytics and Reporting
Advanced EMR platforms offer dashboards and analytical tools. Hospitals can track patient outcomes, physician performance, and disease trends—empowering data-driven decision-making.
8. Secure Access Control
Because medical records contain sensitive data, EMR systems enforce strict role-based access controls. Multi-factor authentication and audit trails are also common features to prevent unauthorized access.
9. Interoperability Capabilities
Although EMRs are often limited to one facility, modern solutions increasingly support HL7/FHIR standards, enabling partial data exchange with other systems and paving the way for integration with EHRs.
10. Mobile and Remote Access
Cloud-based EMRs allow healthcare staff to securely access records from tablets or smartphones. This is particularly valuable for home care, telemedicine, and emergency services.
Benefits of EMR Systems in Healthcare
Understanding the benefits of EMR systems in healthcare helps explain why so many hospitals, clinics, and private practices are adopting digital medical records. Beyond convenience, EMRs drive efficiency, safety, compliance, and patient satisfaction.
1. Improved Accuracy and Reduced Errors
Paper-based systems often lead to illegible handwriting, misplaced files, or incomplete information. EMR systems eliminate these issues by storing data digitally and providing real-time access. Features like e-prescribing and drug interaction alerts significantly reduce medical errors.
2. Greater Efficiency and Productivity
Healthcare staff no longer need to shuffle through physical charts. Instead, doctors, nurses, and administrators can quickly locate information, update records, and generate reports. This reduces administrative burden and allows providers to spend more time with patients.
3. Enhanced Patient Safety
One of the most critical benefits of EMR systems in healthcare is patient safety. By consolidating data on allergies, past treatments, and medications, EMRs help clinicians avoid harmful mistakes and provide better continuity of care.

4. Better Patient Engagement
Many EMR systems are integrated with patient portals, allowing individuals to view lab results, schedule appointments, and message their providers online. This transparency encourages patients to take an active role in managing their health.
5. Seamless Billing and Insurance Processing
With built-in billing modules, EMRs simplify insurance claims, eligibility checks, and coding. This reduces delays in reimbursements and minimizes errors in financial records.
6. Data-Driven Insights
Hospitals and clinics can use EMR analytics to track disease trends, identify at-risk patients, and monitor physician performance. These insights support preventive care, operational efficiency, and long-term planning.
7. Compliance with Regulations
Healthcare organizations face strict requirements such as HIPAA (US), GDPR (EU), APPI (Japan), and PDPA (Singapore). EMR systems are designed to meet these standards, ensuring secure handling of sensitive health information.
8. Cost Savings Over Time
Although implementation requires investment, EMRs reduce costs in the long term by eliminating paper, storage, and redundant processes. They also cut down on duplicated tests and unnecessary procedures.
9. Improved Collaboration
Authorized staff across different departments—doctors, lab technicians, pharmacists—can access the same patient file simultaneously. This fosters better communication and coordinated care.
10. Scalability and Future Readiness
Modern EMR systems are designed to grow with the organization. They can integrate with telehealth platforms, wearable devices, and AI-powered diagnostic tools, ensuring that hospitals are prepared for future digital healthcare trends.
EMR vs. EHR: What’s the Difference?
When exploring what is EMR systems, one of the most common points of confusion is the difference between EMR (Electronic Medical Records) and EHR (Electronic Health Records). While they may sound similar, they serve distinct purposes in healthcare digitalization.
Definition
- EMR (Electronic Medical Record): A digital version of a patient’s chart within a single healthcare facility. Used mainly by doctors and staff for diagnosis and treatment in that clinic or hospital.
- EHR (Electronic Health Record): A broader, interoperable record that can be shared across multiple healthcare organizations. It provides a complete view of a patient’s health history, even if they visit different providers.
Key Differences Between EMR and EHR
| Aspect | EMR (Electronic Medical Record) | EHR (Electronic Health Record) |
|---|---|---|
| Scope | Records within one healthcare facility | Comprehensive health records across multiple facilities |
| Data Sharing | Limited to internal use | Designed for interoperability and nationwide exchange |
| Focus | Clinical use: diagnoses, treatments, prescriptions | Longitudinal health record: includes medical, social, lifestyle data |
| Users | Doctors, nurses, and staff in one clinic/hospital | Multiple providers, insurance companies, labs, specialists |
| Examples of Use | A cardiology clinic managing its patients’ medical files | A national health system allowing any doctor to access full patient history |
| Patient Access | Usually limited | Often includes patient portals for engagement |
Why the Confusion?
The terms EMR and EHR are sometimes used interchangeably by vendors and even governments. In the United States, for example, the Department of Health and Human Services (HHS) often uses “EHR” as the preferred term when discussing national healthcare IT programs, while many providers still say “EMR.”
Which One Should Healthcare Providers Choose?
Small or single-location practices often find EMR systems sufficient for daily operations.
Larger hospital networks, government initiatives, and integrated care systems typically adopt EHRs to ensure data interoperability.
The Bottom Line
- EMR = digital patient chart for internal use.
- EHR = comprehensive, shareable health record across multiple organizations.
Both are critical to the digital future of healthcare, but EHRs represent the next step toward fully connected, patient-centric care.
Types of EMR Systems
Not all healthcare organizations have the same needs. A small private clinic won’t require the same EMR system as a large hospital network. To answer the question “what is EMR systems?” fully, it’s important to explore the different types available today.
1. On-Premises EMR Systems
These are installed locally on a hospital’s or clinic’s servers and maintained by the internal IT team.
Advantages:
- Full control over data storage and security.
- Customizable to unique workflows.
- No reliance on external internet connectivity.
Disadvantages:
- High upfront costs for hardware and licensing.
- Requires continuous IT maintenance and upgrades.
Best for: Large hospitals or institutions with strong IT infrastructure.
2. Cloud-Based EMR Systems
Cloud EMRs are hosted on secure, external servers and accessed through the internet.
Advantages:
- Lower upfront costs compared to on-premises solutions.
- Accessible anytime, anywhere (ideal for telemedicine and multi-location clinics).
- Automatic updates and reduced IT burden.
Disadvantages:
- Dependence on internet reliability.
- Security risks if vendor compliance is weak.
Best for: Small to medium clinics, or providers needing remote access.
3. Specialty-Specific EMR Systems
Designed for particular medical practices such as cardiology, pediatrics, dermatology, dental, or mental health.
Advantages:
- Tailored templates and workflows.
- Specialty-specific features (e.g., dental charting, oncology treatment tracking).
- Higher efficiency for niche practices.
Disadvantages:
- May lack flexibility for general medical use.
- Integration with broader hospital systems can be limited.
Best for: Clinics or specialists with unique requirements.
4. Custom-Built EMR Systems
Developed specifically for a healthcare provider’s unique processes and compliance needs.
Advantages:
- Complete flexibility and customization.
- Can integrate seamlessly with existing hospital systems.
- Future-proof with scalability options.
Disadvantages:
- Higher development cost and longer implementation time.
- Requires choosing a reliable development partner.
Best for: Healthcare organizations with complex or highly specific workflows.
5. Open-Source EMR Systems
Built on community-driven platforms that allow providers to customize and modify freely.
Advantages:
- No licensing fees.
- Flexible customization.
- Supported by global developer communities.
Disadvantages:
- Requires strong internal IT expertise.
- Limited vendor accountability and official support.
Best for: Tech-savvy clinics or organizations with internal developers.
Challenges of EMR Systems
Despite their benefits, EMR systems face several challenges:
- High initial costs (software licensing, hardware, training).
- Interoperability issues (limited data sharing across facilities).
- User resistance from physicians used to paper records.
- Cybersecurity risks due to sensitive patient data.
- Maintenance and upgrades that require skilled IT support.
EMR Systems in Australia, Singapore, and the US
- Australia: My Health Record initiative promotes interoperability across states.
- Singapore: National Electronic Health Record (NEHR) is a unified platform.
- United States: HIPAA and Meaningful Use programs drive EMR/EHR adoption.
These examples show how healthcare systems are moving toward broader digital health ecosystems.
How to Choose the Right EMR System for Your Healthcare Facility
Here are the key factors to consider when choosing an EMR system for your healthcare facility:
1. Compliance with Healthcare Regulations
Ensure the EMR system complies with national and regional healthcare standards such as:
- HIPAA (United States)
- GDPR (European Union)
- APPI (Japan)
- PDPA (Singapore)
Compliance guarantees that patient data will be stored, processed, and transmitted securely.
2. User-Friendliness for Medical Staff
Doctors and nurses should be able to navigate the system quickly without lengthy training. A poor user experience can slow down workflows, reduce adoption rates, and cause frustration.
Tip: Look for systems with customizable dashboards, easy navigation, and voice-recognition capabilities.
3. Integration Capabilities
A good EMR system should integrate seamlessly with:
- Laboratory information systems (LIS)
- Radiology and imaging systems
- Pharmacy systems
- Billing and insurance platforms
- Telemedicine and patient portal tools
Interoperability reduces duplication of work and ensures a smooth data flow across departments.
4. Scalability and Flexibility
Your healthcare facility may expand over time. Choose an EMR system that can scale with your growth—whether that means adding more users, multiple departments, or integration with new technologies like AI or IoT medical device.
5. Data Security and Access Control
Security is critical when handling sensitive patient information. Look for:
- Role-based access controls
- Multi-factor authentication (MFA)
- Audit trails
- Encryption at rest and in transit
This ensures compliance and minimizes risks of data breaches
6. Vendor Reliability and Support
Your relationship with the EMR vendor should be long-term. Evaluate:
- 24/7 technical support availability
- Regular updates and patches
- Customer success programs
- Training resources for staff
7. Cost Structure
Understand the full pricing model, including:
- Upfront costs (licensing, hardware, customization)
- Ongoing costs (subscription fees, maintenance, training)
- Hidden costs (integration, data migration, compliance upgrades)
Balancing budget with long-term ROI is essential.
8. Customization Options
Every healthcare organization has unique workflows. A flexible EMR system allows customization for:
- Specialty templates (e.g., cardiology, pediatrics, dentistry)
- Unique billing codes
- Reporting dashboards
- Patient engagement features
9. Mobility and Remote Access
With telehealth and home care growing, having cloud or mobile access is critical. This ensures doctors can securely access patient data anywhere, anytime.
10. Pilot Testing and Feedback
Before fully rolling out the EMR system, conduct a pilot phase with a small group of physicians and staff. Gather feedback on usability, performance, and workflow impact. This helps identify gaps before large-scale deployment.
HBLAB – Your Trusted Partner for EMR System Development
At this stage, you may not only ask what is EMR systems but also who can build or customize one for your organization?
HBLAB is a global IT outsourcing and AI solution provider specializing in custom EMR development. With proven expertise in healthcare IT, we help clinics and hospitals implement secure, scalable, and cost-effective EMR solutions.
Why Choose HBLAB?
- Global Presence: Headquarters in Vietnam, with branches in Australia, Singapore, Japan, and Korea.
- Large Team: 630+ professionals with strong English communication skills.
- Experienced Talent: 30% senior-level engineers (5+ years in complex projects).
- Flexible Models: BOT (Build Operate Transfer), offshore, onsite, and dedicated team models.
- Cost Advantage: Up to 30% lower cost than local providers.
- Technology Expertise: Diverse programming skills for healthcare solutions.
- Security Compliance: CMMI Level 3 certified, strict adherence to security standards.

Whether you need a custom EMR system, a migration from legacy software, or an AI-powered healthcare solution, HBLAB provides end-to-end services to help your digital transformation succeed.
Conclusion
So, what is EMR systems? Simply put, it is the digital backbone of modern healthcare – a platform that replaces paper charts with accurate, accessible, and secure electronic medical records.
From improving clinical efficiency to enhancing patient safety, EMR systems are indispensable in today’s healthcare landscape. While challenges like cost and interoperability remain, advancements in cloud computing, AI, and security will continue to drive innovation.
If your healthcare organization is ready to embrace the future of digital healthcare, HBLAB is here to help with world-class EMR development and support.
See more:
– Machine Learning – ML vs Deep Learning: Understanding Excellent AI’s Core Technologies
– Healthcare App Development: Revolutionizing Patient Care and Medical Practices
– Healthcare Software Development: 7 Powerful Trends Reshaping Global Care